
World Hepatitis Day
Unmasking Hepatitis: The Silent Liver Destroyer
Hepatitis is an inflammation of the liver caused by a variety of infectious viruses and noninfectious agents. The resulting health problems can be fatal.
Viral Hepatitis — A Global Burden
There are five main strains of the hepatitis virus, referred to as types A, B, C, D, and E — or HVA, HVB, HVC, HVD, and HVE. While they all cause liver disease, they differ in important ways, including modes of transmission, severity of the illness, geographical distribution, and prevention methods. Types B and C, in particular, lead to chronic liver infection in hundreds of millions of people. According to the World Health Organization (WHO), approximately 360 million people worldwide are infected with hepatitis B or C. The ongoing inflammation over years and decades results in severe liver damage, making HAB and HAC the most common causes of liver cirrhosis, liver cancer, and viral hepatitis-related deaths. The WHO estimates that liver cancer rates are set to rise globally by 55% in the next two decades due to the long-term effects of the spread of viral hepatitis.
World Hepatitis Day — Take Action Now!
#WorldHepatitisDay is one of the World Health Organization’s officially mandated global public health days. It is a day when the world comes together to raise awareness of hepatitis, one of the most deadly and neglected health crises, claiming a life every 30 seconds. Globally, over 1.3 million lives are lost each year to hepatitis B and C, more deaths than to HIV or tuberculosis. With only six years left to meet the global goal of eliminating hepatitis by 2030, we are moving backwards. Yet, we have the tools to eliminate the disease and prevent much suffering and death.
How Does Hepatitis Endanger Your Health?
The liver has many important functions in the body: it detoxifies the blood, plays a crucial role in metabolism, digestion, the immune system, and blood clotting. However, long-term hepatitis damages liver cells. Chronic inflammation can cause scarring in the liver tissue, called liver fibrosis. When the liver is severely damaged — a condition known as liver cirrhosis — it can no longer perform its vital functions, leading to liver failure. Detoxification of the body fails, and necessary factors for blood clotting are not sufficiently produced. Additionally, the blood flow through the liver is restricted, causing blood congestion and varicose veins around the stomach and esophagus, with the risk of severe bleeding events. Ongoing inflammation also increases the risk of liver cancer. Liver diseases often go unnoticed for a long time or only cause non-specific symptoms such as fatigue. By the time severe symptoms arise, liver destruction is often advanced, and liver transplantation may be the only option. However, timely diagnosis and treatment of hepatitis can often prevent such serious consequences.
Symptoms of Hepatitis: When to Be Alarmed?
Be informed and pay attention to possible signs of hepatitis. Early detection prevents the spread and can help prevent serious complications. Talk to your doctor if you experience any of the typical signs and symptoms of hepatitis:
-> A few initial days of mild fever, reduced appetite, nausea, and vomiting
-> Abdominal pain, itching, skin rash, or joint pain
-> Jaundice (yellowing of the skin), dark urine, and pale stools
-> A slightly enlarged, tender liver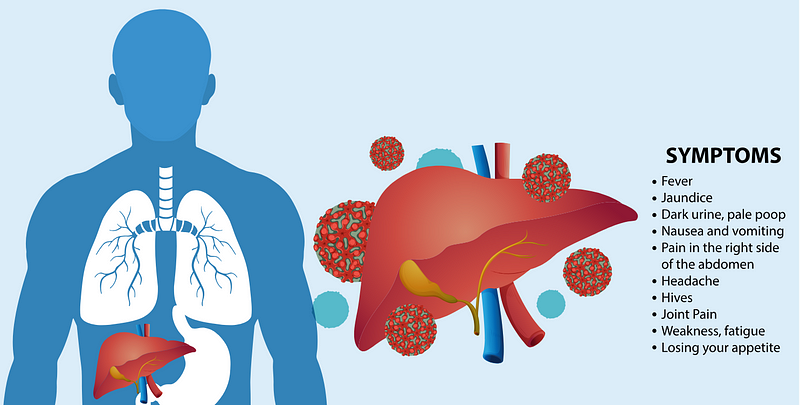
The Alphabet of Hepatitis
The viruses that can cause hepatitis are very diverse and therefore need to be considered separately.
The Hepatitis A Virus (HAV)
was discovered in 1973. It is present everywhere in the world but is uncommon in countries with high standards of hygiene.
Transmission from one person to another is possible if they are in close contact, for example, in a shared household or childcare facility, when virus are spread by smear infection through tiny traces of feces on hands or objects. The HAV is frequently transmitted by eating contaminated foods, such as salads and vegetables that were grown using feces as fertilizer, or seafood, such as mussels or oysters. They can also get into food from unwashed hands, for example, when preparing meals. Dirty drinking water or bathwater can also be a source of infection. Transmission through blood and blood products is also possible.
Symptoms are usually mild in infected children, whereas adults generally become much more ill. The first signs of an infection are nausea, vomiting or stomach pains, a general feeling of illness and, in some cases, a high temperature. Some patients develop jaundice, with yellowing of the skin and conjunctiva, dark urine, pale stools and severe itching of the skin. The symptoms usually last for anything from a few days to several weeks. It normally takes another two to four weeks before the patient makes a full recovery. Chronic courses with HAV are not known, and the infection almost always heals without consequences. However, this process may sometimes take months. Rarely, severe and even fatal events are observed: Especially elderly people and people with chronic liver disease are at risk. Once recovered, patients are immune to HVA for life.
There is no drug therapy for hepatitis A. It is only possible to alleviate symptoms such as vomiting or flu-like symptoms. A vaccine protects against infection with the hepatitis A virus. It is recommended for travel to countries with lower hygiene standards.
The Hepatitis B Virus (HBV)
was identified in 1966 as the first hepatitis virus — seven years before the HVA virus! Until this time the pathogens were not known and “hepatitis A” and “hepatitis B” were only general terms for liver infections transmitted by water (hepatitis aqua) or blood (hepatitis blood).
HBV can be transmitted through blood and other body fluids. Particularly at risk are sexual partners of infected and newborn babies from HBV-positive mothers. Lack of hygiene during medical procedures, piercing or tattoos can also lead to infection. In the drug scene, transmissions are also more frequent due to jointly used utensils.
In adults, a new infection with HBV in 90 to 95% of cases recovers itself within the first six months. In infants, in children and adolescents, and in immunodeficient patients, the prospects for spontaneous recovery are significantly lower.
With spontaneous healing, all the components of the virus disappear from the blood. The only remaining antibodies are in response to the immune system. Healed HBV patients are no longer contagious and usually immune until the end of their lives. However, HBV leaves its hereditary material permanently in the core of the liver cells — even after a spontaneous healing. Therefore, even a “cured” HBV can become active again decades later and pass the immune system when this is severely suppressed, for example, by chemotherapy or rheumatism therapy. However, prophylactic antiviral treatment can prevent reactivation in such situations.
If HBV remains measurable in the blood for more than six months (HBsAg positive), it is chronic and then usually lasts for life. In the long term, a chronic HBV infection can lead to liver cirrhosis and liver cancer in the form of so-called hepatocellular carcinoma (HCC).
Medications are not yet able to cure chronic hepatitis B completely. But they can alleviate severe courses and minimize the risk of liver damage. Research is working on improved hepatitis B therapies.
There is a safe vaccine against HBV. Like the HAV vaccine, it is not contagious and is generally well tolerated.
The Hepatitis C Virus (HCV)
was discovered in 1989. As a rule, blood-to-blood contact is required for its transmission. Until its discovery, blood products were a common source of infection. Today, transmission through the screening of blood donations is almost excluded.
Sharing utensils while using drugs remains a high risk. Infection is also possible due to hygienic defects during piercing, tattooing or medical procedures. Compared to HBV, HCV is less likely to be sexually transmitted, but the risk increases with injuries, menstruation and special practices.
Daily contact with shaking hands, hugging, kissing, or sharing a toilet or food does not transmit HCV.
The World Health Organization estimates that about 30% of HCV infections cure themselves in the first half of the year, but in 70% of cases become chronic. Untreated, chronic HCV can lead to liver cirrhosis after years or decades. Cirrhosis also increases the risk of liver cell cancer. Meanwhile, there is evidence that cardiovascular diseases, strokes and tumors in other organs are also more common in HCV.
Until now, no vaccine has been developed to protect against this virus.
However, HCV is almost always curable today thanks to improved medications. As a rule, today, an eight to twelve weeks of therapy is carried out. 95 to 100% of patients are permanently free of HCV after the first cycle of therapy. A prerequisite is, of course, that patients consistently take their tablets daily. Rarely a second therapy is needed, but then the chances of recovery are similarly high today. Nowadays, almost any HCV infection can be cured. The virus seems to be completely removed from the body after such therapies.
The biggest challenge with HCV now remains that many patients are still undiagnosed. Symptoms often disappear for years or are only non-specific. The global elimination goal for HCV requires both a consistent screening of risk groups and a much greater dissemination of knowledge about the dangers of HCV among doctors and the public.
The Hepatitis D Virus
discovered in 1978, can only occur in conjunction with the HBV, because it is an incomplete virus without its own cover. The transmission can take place through blood and sexual contact, with the HDV either being transmitted simultaneously with HBV or later adding to an existing chronic HBV infection.
Co-infection with HBV and HDV is often more severe and leads to faster liver damage than a single HBV infection. Therefore, HDV is considered to be the most dangerous hepatitis virus known today.
The treatment options for HDV infection are still very limited, they only work in a part of the patients and then mostly temporarily. However, vaccination against HBV also indirectly protects against HDV.
The Hepatitis E Virus (HEV)
is found worldwide, but the disease is most common in East and South Asia. The HEV disease occurs both as outbreaks and as sporadic cases. The outbreaks usually follow periods of fecal contamination of drinking water supplies and may affect several hundred to several thousand persons. Some of these outbreaks have occurred in areas of conflict and humanitarian emergencies such as war zones and camps for refugees or internally displaced populations, where sanitation and safe water supply pose special challenges.
Sporadic cases are also believed to be related to contamination of water, albeit at a smaller scale. The cases in these areas are caused mostly by infection with genotype 1 virus, and much less frequently by genotype 2 virus.
In areas with better sanitation and water supply, HEV infection is infrequent, with only occasional sporadic cases. Most of these cases are caused by genotype 3 virus and are triggered by infection with virus originating in animals, usually through ingestion of undercooked animal meat. These cases are not related to contamination of water or other foods. Sometimes you can also see transmissions from strawberries or other field fruits when fertilized with animal feces.
In the past, there were also infections from blood products, but now blood donors are also tested for HEV to minimize the risk.
In over 99% of cases, HEV heals itself and is sometimes not even felt. However, typical hepatitis symptoms, such as yellowing of the skin and eyes, may occur. Rarely, neurological complications are also possible, such as pain, numbness or even paralysis. Persons with chronic liver diseases are at risk, as an additional HEV infection can worsen their condition and lead to liver failure.
Certain forms of hepatitis E virus, especially genotypes 1 and 2, which are more common in Asia and Africa, can also cause liver failure in pregnant women. Although chronic hepatitis E is rare, untreated, it can lead to liver cirrhosis in a few years.
In Europe and the United States, were the genotype 3 is most prevalent, there is no approved vaccine against HEV, currently. A Chinese vaccine has been developed against genotype1 of HEV.
Hepatitis Vaccination — Small Prick, Life Saving
Some types of hepatitis are preventable through vaccination. A WHO study found that an estimated 4.5 million premature deaths could be prevented in low- and middle-income countries by 2030 through vaccination, diagnostic tests, medicines and education campaigns. WHO’s global hepatitis strategy, endorsed by all WHO Member States, aims to reduce new hepatitis infections by 90% and deaths by 65% between 2016 and 2030.
The Ministry of Health and Prevention (MoHAP) has stressed that eradicating hepatitis has been and will continue to be a top priority for the UAE’s health system. Hence, it has adopted a national initiative to battle the disease, a combined effort by the government and private healthcare sectors. The preventive measures include raising awareness, vaccinating travelers and healthcare workers, and instituting hepatitis B and C screenings for those at greatest risk. This is in addition to implementing screenings during premarital check-ups, residency tests, and occupational health evaluations across the country.
Let’s fight against unnecessary suffering and premature deaths caused by hepatitis!
Take advantage of effective prevention by vaccination!
Stay informed and aware of signs of hepatitis — Contact your doctor in case of symptoms!
Save global lives by stop spreading hepatitis virus!
Comments
Post a Comment